In groundbreaking research published recently, a team of international scientists has shed new light on the dynamic interplay between the hepatitis B virus (HBV) and its human hosts. By conducting an extensive “genome-to-genome” analysis involving 567 individuals living with chronic hepatitis B, the study sought to untangle the intricate evolutionary adaptations of the virus in response to host genetic pressures. The primary focus lay on detecting any consequential genomic correlations between human genetic variations and viral mutations.
The researchers successfully identified a significant link between a common genetic variant in East Asians in the NTCP gene, the receptor HBV uses to enter liver cells, and specific mutations in the virus’s preS1 region, which is critical for binding to this receptor. Notably, these mutations appear to enhance the virus’s ability to bind to the mutated NTCP receptor, potentially easing its entry into hepatocytes.
Moreover, the study also revealed intriguing associations between human HLA class I molecules, which play a pivotal role in immune recognition, and certain viral mutations within the epitopes targeted by these molecules. These findings suggest that HBV may evolve to escape the immune system by altering how it interacts with these crucial immune system components.
This research not only deepens our understanding of HBV-host interactions but also opens new avenues for targeted therapeutic interventions, potentially leading to more effective treatments for chronic hepatitis B.
Chronic hepatitis B remains a significant global health challenge, impacting millions of people worldwide and presenting major complications, such as liver cirrhosis and hepatocellular carcinoma. Despite the availability of preventative vaccines and therapeutic drugs, the hepatitis B virus (HBV) persists as a leading cause of liver disease, due in large part to its ability to evolve and adapt within its host. This adaptability not only aids the virus in evading the host’s immune system but also complicates efforts to design universally effective treatments and vaccines.
HBV has a remarkably compact genome, consisting of just over 3,000 base pairs encoding multiple overlapping open reading frames. This genetic efficiency confers a capacity for rapid mutation and evolution, particularly when under immunological or pharmacological pressure. Previous studies have established the reciprocal evolution of the virus in the presence of host immune responses. However, the specific interactions between host genetics and viral sequences have been less thoroughly examined, with past research often focusing only on either viral or host genetic factors in isolation.
This latest research is pivotal as it integrates comprehensive genomic data from both the virus and its hosts, exploring how different genetic backgrounds can influence viral behavior and susceptibility to infection. The study’s focus on a genome-to-genome approach is particularly innovative, as it goes beyond traditional single-angle studies to map the complex web of genetic interactions.
East Asian populations, where certain HBV strains and specific human genetic traits predominate, present a unique opportunity for such research. The prevalence of the HBV surface antigen in these populations is among the highest globally, often exceeding 8-10%. This regional specificity makes the genetic correlations identified in the NTCP gene particularly relevant.
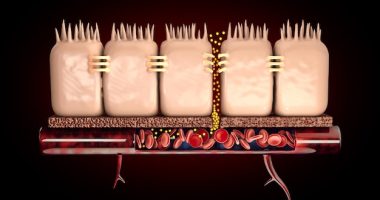
The NTCP (sodium taurocholate co-transporting polypeptide) gene encodes a receptor on hepatocytes that is crucial for HBV entry into liver cells. Variations in this gene in different populations may impact the effectiveness of the virus’s entry mechanism, thereby influencing infection rates and disease progression. The highlighted interaction between host NTCP variants and viral mutations in the preS1 region of HBV, which facilitates binding to hepatocytes, suggests a direct evolutionary response by the virus to optimize its infectious capabilities against altered cellular landscapes.
Moreover, the study’s insights into the interaction between human HLA class I molecules and the virus underscore the ongoing arms race between HBV and human immune defenses. HLA molecules play essential roles in presenting viral peptides to immune cells, prompting targeted immune responses. The identified viral mutations within these epitopes offer a glimpse into how HBV changes its surface proteins to evade immune detection and destruction.
Continuing to unravel these complex genetic interplays will be crucial for the next steps in HBV research and treatment development, offering the potential for personalized therapies that take into account both viral characteristics and host genetic factors. Such precision medicine approaches could revolutionize the management of chronic hepatitis B and potentially other infectious diseases by making treatments more effective and reducing the risk of drug resistance.
To unveil the genomic interactions between the hepatitis B virus (HBV) and its human hosts, the research team employed a comprehensive “genome-to-genome” analysis approach. This methodology was painstakingly designed to capture and compare the genetic details of both the virus and the infected individuals to identify correlations that could influence the course of the infection and the effectiveness of the immune response.
### Participant Selection and Data Collection
The study involved 567 participants diagnosed with chronic hepatitis B from diverse geographic and ethnic backgrounds, specifically focusing on populations in East Asia where HBV is highly prevalent. The team ensured a balanced representation of genetic backgrounds to avoid biases in genetic variability. Each participant provided blood samples from which DNA was extracted. These samples were then subjected to rigorous genome sequencing to decode both the human and viral genomes.
### Genome Sequencing and Analysis
For human genomes, researchers utilized high-throughput sequencing technologies that allowed for detailed mapping of individual genetic variations, particularly focusing on single nucleotide polymorphisms (SNPs) linked to differences in disease susceptibility and progression. For the viral genome, the team used specialized viral sequencing techniques capable of capturing the fast-mutating HBV genome, which presents significant challenges due to its high variability and overlap in genetic coding sections.
The sequencing data underwent extensive bioinformatics analysis to align and compare sequences from the virus and the hosts. The focus was on identifying mutational patterns in the virus that correlated with specific human genetic variations. Particular attention was given to mutations in the viral preS1 region and their association with variants in the human NTCP gene, as well as changes in viral epitopes related to human HLA class I molecules.
### Statistical Modeling and Correlation Analysis
To determine the significance of the observed genetic correlations, the team employed sophisticated statistical models. These models were designed to filter out background noise and pinpoint genuine associations between host genetic factors and viral adaptations. They controlled for potential confounders such as age, sex, duration of infection, and other clinical factors that might influence the outcomes.
### Verification and Validation
The findings from the initial analysis were subjected to rigorous validation steps. This involved replicating the study with additional cohorts where feasible and performing in vitro experiments to observe the interaction between the viral mutations and host receptor proteins in a controlled environment. These experiments helped confirm the biological relevance of the genomic correlations identified, particularly how mutations affect the virus’s ability to enter liver cells and escape immune surveillance.
### Conclusion of Methodology
This integrated genome-to-genome analysis approach provided a comprehensive understanding of the co-evolutionary battles between HBV and its human hosts. By combining detailed genomic sequencing with advanced bioinformatics and statistical analysis, the research not only highlighted specific evolutionary adaptations of the virus but also paved the way for developing targeted therapies that consider both viral and host genetic factors. This methodology stands as a model for studying other complex virus-host interactions and can significantly impact the development of personalized medical strategies in infectious disease management.
### Key Findings and Results
Through the meticulous genome-to-genome analysis carried out by the research team, several crucial discoveries emerged regarding the interaction between the hepatitis B virus (HBV) and the genetic makeup of its human hosts. One of the most significant findings was the identification of a strong correlation between a common genetic variant in the NTCP gene, prevalent in East Asians, and specific mutations in the HBV preS1 region. The preS1 region of the virus is crucial for its ability to bind to the NTCP receptor on hepatocytes—the liver cells that the virus infects. The identified mutations in the preS1 region potentially increase the virus’s binding affinity, suggesting a direct viral adaptation to enhanced receptor availability, thereby facilitating easier viral entry and possibly influencing infection severity and treatment outcomes.
Furthermore, the study also highlighted a dynamic interaction between HBV and the human immune system, marked by an evolutionary tug-of-war. Specifically, the team found correlations between human HLA class I molecules, which are pivotal in immune response, and certain viral mutations within the HBV epitopes. These epitopes are essentially portions of the viral protein presented by HLA molecules on the surface of cells to T-cells, triggering an immune response. The mutations in these epitopes suggest that HBV can alter its physical presentation to evade immune detection, a strategy that could undermine the efficacy of immune-based therapies and natural immune surveillance.
Another notable result involved the broader implications of the interplay between host genetic variants and the HBV genome. Certain human genetic profiles were associated with differences in viral load and disease progression, indicating that host genetics not only influence susceptibility to infection but also the clinical trajectory of the disease. This finding is critical as it implies that patient-specific genetic factors could be integrated into treatment plans, potentially tailoring interventions to improve therapeutic efficacy.
In addition to identifying genetic interactions, the research provided insights into potential new therapeutic targets. For instance, the interaction between viral mutations and the NTCP receptor suggests that blocking these interactions might prevent the virus from entering liver cells, offering a strategy for therapeutic intervention. Similarly, understanding how HBV evades immune detection by mutating viral epitopes can lead to the design of vaccines or therapies that aim to restore effective immune recognition.
Finally, the geographical and ethnic diversity of the study participants, particularly from regions with high HBV prevalence, enabled the researchers to validate their findings across different genetic backgrounds, enhancing the global relevance of the results. This comprehensive approach aids in understanding how genetic diversity influences disease dynamics, which is essential for developing universal as well as region-specific strategies to combat HBV.
### Implications and Future Directions
The implications of these findings extend beyond the realm of hepatitis B research. They underscore the crucial role of a detailed genetic understanding in tackling viral diseases, which could revolutionize treatment approaches not only for HBV but also for other persistent viral infections. The methodology developed and applied in this study provides a blueprint for future research where multi-genomic data integration can uncover precise mechanisms of pathogen-host interactions.
Going forward, these findings beckon additional studies to further dissect the identified correlations and to translate these insights into clinical practice. The potential for developing precision medicine approaches that incorporate both viral characteristics and host genetic factors could significantly change the landscape of chronic hepatitis B management and pave the way for customized therapeutic regimens. Moreover, the research opens avenues for exploring similar genomic interactions in other viral diseases, potentially leading to breakthroughs in infectious disease control and prevention.
### Implications and Future Directions
The groundbreaking findings from this comprehensive “genome-to-genome” analysis herald a new era in the fight against chronic hepatitis B, opening up promising avenues for personalized medicine that could transform patient care and therapeutic outcomes. By pinpointing the genetic interplay between the hepatitis B virus and its human hosts, researchers have unlocked a deeper understanding of how genetic variations in both the virus and the host contribute to disease dynamics. This understanding is crucial for the development of targeted therapies and vaccines that can effectively counter the virus’s tactics to evade immune detection and leverage host receptors for entry.
One of the most immediate applications of these findings will be in the improvement of antiviral therapies. The identification of key interactions between the virus’s preS1 region and human NTCP receptors paves the way for designing inhibitors that can block these interactions and prevent the virus from entering liver cells. Furthermore, the insights into how HBV mutates to escape immune surveillance can direct the development of more robust vaccines that can anticipate and counteract these mutations.
Moreover, the regional and ethnic diversity included in this study underlines the significance of genetic context in disease management. This diversity allows for the extrapolation of the findings across different populations, which is vital for the creation of global health strategies as well as tailored local solutions. Given the varying prevalence and genetic profiles worldwide, region-specific treatment and prevention strategies could be developed based on a deep genetic understanding.
Looking to the future, this research model can be extended to other viral infections where host-pathogen interactions play a crucial role in disease progression and treatment outcomes. Diseases like HIV, influenza, and even emerging viral threats could be studied under this lens, potentially leading to significant breakthroughs in how these diseases are managed and controlled. The integration of host genomic data with pathogen genomic data, as demonstrated in this study, suggests a blueprint for a multi-genomic approach to infectious disease research and treatment.
Furthermore, ongoing research will need to explore the longitudinal impact of these genetic interactions on disease progression and treatment responses over time. Long-term studies that track patients from diagnosis through treatment could provide invaluable data on how genetic factors influence the trajectory of hepatitis B and help refine treatment protocols based on patient-specific genetic and viral profiles.
As we move forward, collaboration across disciplines and borders will be essential to harness the full potential of these findings. Partnerships between geneticists, virologists, clinicians, and pharmaceutical industries will play a critical role in translating these scientific insights into practical, effective medical solutions. Moreover, an increased focus on educating healthcare providers and patients about the genetic factors influencing HBV infection could improve decision-making and support the implementation of personalized treatment plans.
In conclusion, the implications of this research are profound, promising to usher in a new paradigm in the management of not only hepatitis B but potentially other chronic viral infections as well. As we continue to unravel the complex genetic codes that govern virus-host interactions, our ability to combat these pervasive diseases will increasingly become more precise, more personalized, and, hopefully, more effective. The future of infectious disease treatment and prevention lies in the continued exploration and application of genome-to-genome analyses, which is set to redefine our approach to combating viral pathogens in the 21st century.