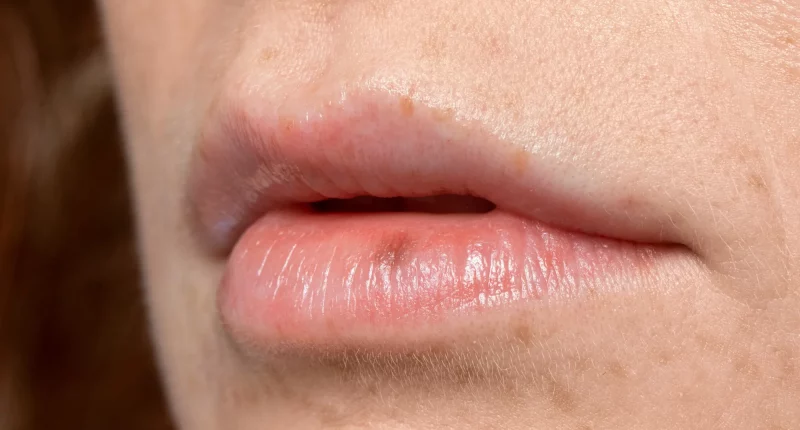
Cheilitis is a condition where the skin on your lips becomes dry, red, flaky, and itchy. It can be caused by various factors, including allergies, infections, irritants, or even habits like licking your lips frequently.
To diagnose cheilitis, a healthcare provider will review your medical history and examine your lips and mouth. If the cause is unclear or if they suspect an allergy, inflammatory disease, or cancer, they might perform additional tests such as patch testing or a skin biopsy. Treatment for cheilitis will depend on what is causing the problem.
Symptoms
Cheilitis presents with several common symptoms across its different kinds. These include dryness of the lips, redness, and swelling. Individuals may also experience peeling or scaling of the lip skin, along with cracking or splitting. Sensitiveness, burning, and itching sensations are often reported. Additionally, crusting at the mouth corners and changes in lip color can occur.
If cheilitis is not properly treated, it can cause secondary infections. Bacteria may enter abrasions or cracks in the skin, causing infections that could result in permanent discoloration, scarring, and lip thickening.
Types and Causes
Cheilitis involves inflammation, which is the body’s natural reaction to infection, injury, or disease. This inflammation causes pain, swelling, warmth, and redness in the affected tissues.
Eczematous Cheilitis
The most common type of cheilitis is eczematous cheilitis, where atopic dermatitis, or eczema, affects the lips. This non-contagious condition arises from an abnormal defense system. It is particularly prevalent among individuals with other atopic conditions, such as food allergies, hay fever, and asthma. Symptoms of eczematous cheilitis can be triggered by irritants or allergens and may persist for up to three weeks. Common triggers include lip balms or lipstick, mouthwash or toothpaste, food allergens, latex or rubber, metals like nickel and gold, sunscreen, particular topical medicines such as bacitracin, food additives such as propylene glycol, persistent lip-licking, and dry, cold temperatures.
Actinic Cheilitis
It also known as solar cheilitis, is led by prolonged sun exposure and is frequent on the lower lip. It is considered a precancerous condition and, in rare cases, can develop into squamous cell carcinoma, a kind of skin cancer. This condition predominantly impacts light-skinned individuals who stand for extended periods in the sun without adequate protection. It is also seen in individuals who do work outdoors for hours, such as those in forestry, fishing, or construction industries.
Angular Cheilitis
It affects the corners of the mouth, where saliva collects. When this saliva dries, it takes moisture from the epidermis, causing it to become cracked and dry. This type of cheilitis often involves secondary infections, like those caused by the fungus Candida albicans (leading to oral thrush) or the Staphylococcus aureus (causing infections). It usually resolves within 14 days with treatment but can persist if left unmedicated. Certain individuals are more susceptible, including those with diabetes, vitamin B or iron deficiencies, and denture wearers. Medicines that cause cracks, such as isotretinoin, and children who suck their thumbs, or lick their lips in winter are also at higher chance.
Diagnosis
To diagnose cheilitis, your doctor will start by reviewing your medical history, involving any exposure to foods, cosmetics, irritants, or allergens. They will then conduct a detailed examination of your lips and mouth.
Depending on the primary findings, additional tests may be recommended. These tests can include:
- Skin Prick Test: Small amounts of common antigens are placed just beneath the surface of your skin to check for allergic reactions.
- Patch Testing: A compress containing common antigens is applied to a part of your skin that hasn’t been exposed to the allergen. This helps determine if you have an allergic reaction.
- Punch Biopsy: A small piece of tissue is removed from your lip using a spring-loaded punch. This tissue is examined in a lab to check for abnormalities, including precancerous or cancer conditions.
- Lip Swab: A cotton swab is used to collect skin cells and fluid from the affected area of your lips. This sample is then analyzed in a lab to detect infections through gene-based bacterial and viral cultures or PCR tests.
Cheilitis Treatment
Cheilitis can often be treated effectively, though the approach depends on its basic cause.
Eczematous Cheilitis
For eczematous cheilitis, topical corticosteroids are commonly prescribed. These steroids, applied directly to the lips, help reduce inflammation. To keep the lips moisturized and combat dryness, using an emollient or lip balm, such as petroleum jelly, is beneficial. Additionally, applying an unprescribed antibiotic cream, like Neosporin, can assist prevent secondary infections. It is crucial to avoid identified allergens or irritants and to adopt behavioral modifications, like refraining from lip-licking, to prevent further irritation.
Actinic Cheilitis
The treatment options for actinic cheilitis vary based on their seriousness. These include:
- Surgical Excision: Removing the affected skin lesion alongside a scalpel.
- Cryotherapy: Using extreme cold to remove the affected skin.
- Laser Ablation: Employing a laser to eliminate the damaged skin.
- Photodynamic Therapy: Applying topical substances that react to ultraviolet light to decrease the lesion.
- Topical Chemotherapy: Using cancer-fighting drugs like fluorouracil to destroy abnormal cells.
- Topical Immunotherapy: Utilizing drugs like imiquimod to activate the immune system and halt the growth of premalignant cells.
Angular Cheilitis
Treatment for angular cheilitis typically involves using a topical antifungal to address any yeast infections and a topical bacterial or antibiotic infection. Applying a protective barrier cream or lip balm, like petroleum jelly or zinc oxide, can also be helpful. Improving oral hygiene, including daily cleaning of dentures, is important. If deficiencies in iron or vitamin B are found, supplements may be prescribed.
Summary
Cheilitis is an inflammatory condition affecting the lips, characterized by symptoms like dryness, redness, and cracking. Treatment depends on the cause: eczematous cheilitis is often managed with topical corticosteroids, moisturizers, and avoidance of irritants; angular cheilitis requires antifungal or antibiotic treatments and improved oral hygiene; actinic cheilitis, caused by sun exposure, may need surgical, cryotherapy, laser, photodynamic, topical chemotherapy, or immunotherapy options. Diagnosing cheilitis involves reviewing medical history and may include tests like patch testing, skin prick tests, lip swabs, or biopsies.