Bronchorrhea is when the lungs produce an unusually large amount of watery mucus, leading to a productive cough. To diagnose bronchorrhea, healthcare providers look for the daily coughing up of at least 100 cc of fluid from the lungs, which equals almost twenty teaspoons.
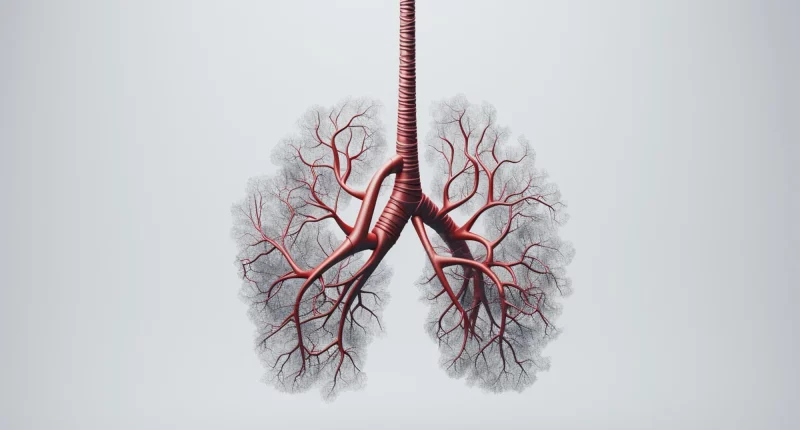
There are various causes of bronchorrhea, with lung cancer being one of the most frequent. More mucus can also signal conditions like bronchiectasis, bronchitis, and other issues affecting the bronchial tubes that are associated with the lungs.
This article explores the causes and symptoms of bronchorrhea. It discusses treatments aimed at addressing the underlying reasons for excessive mucus production and reducing the number of secretions.
Symptoms
Bronchorrhea presents as a condition where significant quantities of thin mucus are expelled from the lungs daily. It’s more than just normal mucus that helps keep the airways moist and clear. Typically, bronchorrhea is most troublesome in the morning and tends to get better as the day progresses.
Individuals with bronchorrhea often experience a continuous cough as their body tries to clear the excessive mucus from their airways. This can lead to feelings of breathlessness because the mucus blocks the passage of air in and out of the lungs. These symptoms can be particularly challenging because they may worsen existing respiratory issues, making it harder to breathe comfortably.
Bronchorrhea isn’t a condition on its own but rather a symptom of underlying health problems. It can exacerbate other conditions that also cause coughing and difficulty breathing, adding to the overall discomfort and impact on daily life.
Complications
Complications from bronchorrhea mainly involve the inconvenience of excessive mucus production, which can be quite significant. However, it can lead to dehydration and imbalances in electrolytes in the body. Severe cases of bronchorrhea might even cause blockages in the airways, leading to respiratory distress and breathing troubles.
Managing bronchorrhea involves addressing the underlying causes to reduce mucus production and alleviate its effects on the body’s hydration and electrolyte levels. This helps in preventing more serious complications and improves overall respiratory function and comfort.
Diagnosis
Diagnosing bronchorrhea typically begins with a thorough medical history and a detailed physical examination. These initial steps help healthcare providers understand the symptoms and assess any potential underlying conditions. In addition to these evaluations, imaging studies like magnetic resonance imaging, computed tomography, or positron emission tomography scans may be ordered. These imaging techniques provide detailed pictures of the lungs and surrounding structures, helping to identify any abnormalities or sources of excessive mucus production.
Furthermore, testing for tuberculosis (TB) is often included in the diagnostic process to eliminate infectious causes that could contribute to bronchorrhea. This involves specific tests designed to detect the presence of TB bacteria or antibodies in the body. Additionally, pulmonary function tests may be conducted to evaluate how well the lungs are functioning and to assess any impairment in respiratory function.
By combining these diagnostic approaches, healthcare providers can gather comprehensive information to pinpoint the underlying cause of bronchorrhea. This enables them to tailor an appropriate treatment plan that targets the specific condition responsible for excessive mucus production, promoting effective management and symptom relief for the patient.
Causes
Bronchorrhea can stem from various underlying conditions, although it is fortunately not very common. One primary group of causes includes chronic respiratory and lung diseases. These conditions encompass a range of disorders affecting the lungs and airways. Chronic bronchitis, a type of chronic obstructive pulmonary disease, is identified by persistent inflammation, which can lead to excessive mucus production. Another condition, bronchiectasis, often results from childhood respiratory infections, causing the airways to widen and collect mucus. Additionally, cough-variant asthma, a form of asthma where the main symptom is a persistent cough, can also contribute to bronchorrhea.
Another significant cause of bronchorrhea is lung cancer, particularly a type formerly known as mucinous bronchioloalveolar carcinoma, now classified under lung adenocarcinoma. This form of cancer is notable for causing excessive phlegm production, affecting about 6% of those diagnosed. Infectious diseases like tuberculosis, though less common in the United States, have also been linked to bronchorrhea.
Beyond respiratory conditions and infections, certain poisonings and stings can induce bronchorrhea. Exposure to organophosphates, which are anticholinesterase pesticides, can lead to severe cases of excessive mucus secretion. Additionally, scorpion stings have been known to provoke bronchorrhea in some cases. Identifying the specific cause of bronchorrhea is crucial for effective management and treatment tailored to address the underlying condition responsible for excessive mucus production.
Treatment
Treating bronchorrhea focuses on addressing its underlying cause, particularly in cases linked to conditions like lung cancer. Understanding how bronchorrhea develops is crucial for choosing the most effective treatment methods.
Unlike typical mucus production associated with lung inflammation, bronchorrhea involves an abnormal hyper-responsiveness of the airways to specific triggers. This distinguishes it from ordinary coughing up of phlegm. Because of this unique mechanism, traditional treatments aimed at reducing general mucus production may not effectively alleviate bronchorrhea symptoms.
Many treatment alternatives are available to manage bronchorrhea, although they generally provide moderate relief. Nonsteroidal anti-inflammatory inhalers and Steroid medications are among the options used to target inflammation and reduce mucus production. Macrolide antibiotics such as clarithromycin and azithromycin are also prescribed to combat infections that may exacerbate bronchorrhea symptoms. Additionally, medications like octreotide, a synthetic hormone, have shown potential in managing excessive mucus secretion in some individuals. Tyrosine kinase inhibitors like gefitinib, typically used to treat lung cancer, have been effective in controlling bronchorrhea by addressing underlying tumor-related mechanisms.
Tailoring treatment to the specific cause of bronchorrhea is essential for improving symptoms and enhancing the quality of life for those affected by this condition.
Summary
Bronchorrhea is characterized by excessive thin mucus production from the lungs, often associated with conditions like lung cancer, chronic lung diseases, and infections. Diagnosis involves thorough medical history, physical exams, and imaging tests to identify underlying causes. Treatment focuses on addressing these causes, such as using steroids, antibiotics, and specialized medications like octreotide and tyrosine kinase inhibitors.
Traditional methods for reducing mucus may not effectively manage bronchorrhea due to its unique mechanism. Managing bronchorrhea requires a tailored approach to alleviate symptoms and improve respiratory function. Understanding the distinct nature of bronchorrhea helps in implementing targeted therapies for better patient outcomes.
External links