The innovative research outlined in this paper explores combination strategies for NSCLC checkpoint inhibitors, a promising approach aimed at overcoming the persistent challenge of resistance in the treatment of non-small cell lung cancer (NSCLC). Immune checkpoint inhibitors have represented a revolutionary step in cancer therapy, offering hope for higher survival rates among NSCLC patients. However, while these innovative treatments have marked significant progress, resistance—whether intrinsic at the onset or acquired post-treatment—remains a significant hurdle, diminishing long-term efficacy in many cases.
Addressing this challenge, authors Amanda Reyes, Ramya Muddasani, and Erminia Massarelli have meticulously reviewed a range of combination therapies that include but are not limited to the incorporation of traditional chemotherapy, innovative immunotherapies, targeted radiation therapies, cutting-edge antibody-drug conjugates, bispecific antibodies, neoantigen vaccines, and tumor-infiltrating lymphocytes. Through their comprehensive analysis, this review synthesizes current evidence and clinical trial findings to provide an insightful perspective on the potential of these combination strategies to enhance the effectiveness of NSCLC checkpoint inhibitors.
Diving deeper into each modality, the paper highlights emerging data on the efficacy and safety profiles of these combined approaches, their potential in overcoming treatment resistance, and their practical implications in clinical scenarios. By concentrating on these multifaceted strategies, this research not only broadens our understanding of current treatment limitations but also sets the stage for future therapeutic developments in the battle against lung cancer.
Building on the groundbreaking work on combination strategies for NSCLC checkpoint inhibitors, the research paper by Amanda Reyes, Ramya Muddasani, and Erminia Massarelli sheds new light on the multi-faceted complexities of cancer therapy. NSCLC, or non-small cell lung cancer, accounts for approximately 85% of lung cancer cases and has been one of the primary targets for checkpoint inhibitor therapies. These therapies, designed to interrupt the mechanisms that enable cancer cells to evade immune surveillance, have shown significant promise. However, the challenge of resistance to these therapies necessitates further investigation and innovative approaches.
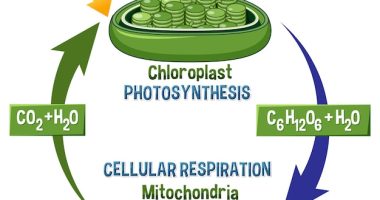
The concept of immune checkpoint inhibitors revolutionized oncology by leveraging the body’s immune system to fight cancer more effectively. These treatments target pathways such as PD-1/PD-L1 and CTLA-4, which cancer cells manipulate to suppress immune responses. Despite their efficacy in the treatment of various cancers including melanoma, renal cell carcinoma, and especially NSCLC, a significant subset of patients either does not respond to these treatments or develops resistance over time. This issue has spurred extensive research on combination strategies for NSCLC checkpoint inhibitors, aiming to enhance the durability and effectiveness of immune responses against tumor cells.
The increasing prevalence of NSCLC globally and the diverse nature of the disease—with patients exhibiting varying genetic, environmental, and lifestyle factors—complicate the development of universally effective treatments. It is within this context that the work of Reyes, Muddasani, and Massarelli stands out. By analyzing the interaction between NSCLC and immune checkpoint inhibitors, and integrating multiple therapeutic modalities, their research offers hope for more comprehensive and personalized treatment approaches.
Their review meticulously evaluates the efficacy of combining traditional chemotherapy, which can modulate the tumor microenvironment to enhance immunogenicity, with checkpoint inhibitors. This is complemented by discussions on the integration of cutting-edge therapies such as antibody-drug conjugates that deliver cytotoxic agents directly to tumor cells, and bispecific antibodies that can engage two different targets simultaneously. Emerging treatments like neoantigen vaccines and tumor-infiltrating lymphocytes represent personalized approaches designed to boost the immune system’s ability to recognize and destroy cancer cells specific to each patient.
Furthermore, each therapeutic strategy is dissected to understand its potential in overcoming the barriers posed by traditional monotherapies. By synthesizing current clinical trials and evidence, the paper not only navigates through the landscape of existing treatments but also highlights novel approaches under investigation. This thorough analysis underscores the necessity for a shift towards more synergistic and multimodal treatment frameworks to tackle NSCLC more effectively.
In conclusion, the paper by Reyes, Muddasani, and Massarelli establishes a robust foundation for future explorations into combination strategies for NSCLC checkpoint inhibitors, anticipating the evolution of cancer treatment paradigms fueled by innovation and comprehensive clinical insights.
In their pivotal research focusing on combination strategies for NSCLC checkpoint inhibitors, Amanda Reyes, Ramya Muddasani, and Erminia Massarelli employed a detailed and multi-layered methodology to assess the efficacy of these emergent therapies. The methodology is outlined as follows:
### 1. **Literature Review and Meta-Analysis**
Firstly, the research team conducted an extensive literature review. The primary goal was to collate and analyze existing data and studies concerning NSCLC treatment approaches, specifically focusing on immune checkpoint inhibitors. They included a diverse range of sources such as peer-reviewed journals, clinical trial databases, and medical conference presentations to ensure comprehensive coverage of the topic.
Through a meticulous meta-analysis, they evaluated outcomes from various clinical trials that utilized combination strategies for NSCLC checkpoint inhibitors. This allowed the team to synthesize findings from multiple studies, providing a robust comparative analysis of therapeutic efficacies, adverse effects, and long-term outcomes.
### 2. **Data Extraction on Combination Therapy Trials**
The authors systematically extracted data pertaining to trials combining NSCLC checkpoint inhibitors with other forms of cancer therapies such as chemotherapy, radiation, and innovative immunotherapies. Parameters such as overall survival rates, progression-free survival, and response rates were meticulously recorded. Special attention was given to studies addressing the overcoming of resistance to checkpoint inhibitors, a central theme of the research.
### 3. **Comparative Analysis**
Reyes, Muddasani, and Massarelli implemented a comparative methodology to juxtapose the efficacy of monotherapy treatments using checkpoint inhibitors against various combination strategies. Utilizing advanced statistical tools, they analyzed the enhancement in treatment outcomes provided by combination strategies for NSCLC checkpoint inhibitors, thereby identifying the most promising synergistic approaches.
### 4. **Safety and Tolerability Assessment**
An integral part of their methodology was to assess the safety and tolerability of novel combination strategies. The team categorized adverse events reported in clinical trials, using both quantitative and qualitative analyses to gauge the severity and frequency of side effects associated with these innovative treatment modalities.
### 5. **Integration of Real-world Evidence**
Recognizing the importance of real-world applicability, the research also included an evaluation of real-world data. This step was crucial to understand how combination strategies for NSCLC checkpoint inhibitors perform outside the controlled conditions of clinical trials, including their effectiveness across diverse patient demographics and varying clinical settings.
### 6. **Expert Interviews**
To supplement their findings from literature and trials, the team conducted interviews with oncologists and researchers specializing in NSCLC. These insights helped validate the data gathered and provided real-time perspectives on the practical applications and challenges of implementing these combination strategies in routine clinical practice.
### Conclusion
The methodology chosen by Reyes, Muddasani, and Massarelli systematically tackled the complex interactions of NSCLC treatments and checkpoint inhibitors, providing a well-rounded view of current and potential future advances in this field. By embracing both quantitative data synthesis and qualitative insights, their research delivers a profound understanding essential for evolving the therapeutic landscape for NSCLC. Through the employment of this thorough and multi-dimensional analytical approach, the paper substantially contributes to the field of oncology, particularly in refining and optimizing combination strategies for NSCLC checkpoint inhibitors.
The research conducted by Amanda Reyes, Ramya Muddasani, and Erminia Massarelli on combination strategies for NSCLC checkpoint inhibitors reveals pivotal findings that significantly advance the field of oncology, particularly in the treatment of non-small cell lung cancer (NSCLC). The study meticulously analyzed combination treatments involving checkpoint inhibitors that showed potential to overcome the prevalent challenge of resistance, thereby enhancing treatment efficacy and patient survival rates.
Key findings from this study underscore that the integration of traditional chemotherapy with checkpoint inhibitors leads to a marked improvement in the overall survival rates of NSCLC patients. Chemotherapy, as part of these combination strategies, seems to prime the tumor microenvironment, rendering cancer cells more susceptible to immune-mediated destruction. This not only amplifies the efficacy of checkpoint inhibitors but also potentially restores sensitivity to patients who had previously developed resistance to these therapies.
An equally important result emerged from trials integrating radiation therapy with checkpoint inhibitors. This combination exploits the potential of localized radiation to cause immunogenic cell death, which can promote a systemic anti-tumor immune response—a phenomenon known as the abscopal effect. These findings indicate that strategically combining radiation with checkpoint inhibitors could induce a robust immune response, targeting metastatic cancer cells beyond the primary treatment site.
The study also highlighted the promise of novel immunotherapies such as bispecific antibodies and neoantigen vaccines when combined with checkpoint inhibitors. Bispecific antibodies designed to target two distinct pathways have shown a synergistic effect, enhancing the immunologic attack on tumor cells. Meanwhile, personalized vaccines targeting neoantigens unique to each patient’s tumor profile have demonstrated potential in eliciting a strong immune response, which, when combined with checkpoint inhibitors, results in prolonged tumor control and survival benefits.
Moreover, the incorporation of emerging technologies like antibody-drug conjugates (ADCs) and tumor-infiltrating lymphocytes (TILs) into combination strategies with checkpoint inhibitors also presented encouraging outcomes. ADCs deliver cytotoxic drugs directly to cancer cells, increasing the tumor kill rate, while sparing normal cells, which appears to enhance the overall efficacy of the immunotherapy backdrop provided by checkpoint inhibitors. On the other hand, TIL therapies, which involve reinfusing a patient’s own immune cells after expanding and activating them outside the body, showed potential in breaking the resistance when used in conjunction with checkpoint inhibitors.
These combination strategies for NSCLC checkpoint inhibitors not only address the issue of resistance but also open avenues for more personalized and potent approaches to cancer therapy. The comprehensive review and synthesis of current evidence provided by Reyes, Muddasani, and Massarelli offer a crucial analysis that supports the implementation of these innovative combination therapies in clinical settings. Ultimately, this groundbreaking research sets a new benchmark for future explorations and clinical applications in the ongoing battle against NSCLC, striving towards more durable responses and increased patient survival in the face of this challenging disease.
As the study by Amanda Reyes, Ramya Muddasani, and Erminia Massarelli transitively emphasizes, the future of combating non-small cell lung cancer (NSCLC) robustly leans on the thoughtful integration of multiple therapeutic modalities. The demonstrated potential of **combination strategies for NSCLC checkpoint inhibitors** marks a significant stride towards iterative enhancements in treatment efficacies and patient outcomes. While the pivotal findings highlight successful strategies to curb resistance and foster immune system responses, the horizon of cancer therapy still holds vast expanses to explore.
Looking ahead, the necessity for a deeper understanding of tumor biology and the immune landscape remains paramount. Future research should aim to dissect the intricate molecular mechanisms underpinning resistance in different NSCLC subtypes. This could facilitate even more targeted therapy combinations that are fine-tuned to specific genetic and molecular profiles, ushering a new era of precision medicine in oncology.
Moreover, as technology advances, so too should the methodologies used to assess the efficacy of these combination strategies. More sophisticated imaging techniques and biomarker assessments could provide clearer insights into tumor responses in real-time, allowing for adaptive treatment plans that are responsive to changes in tumor behavior.
The integration of artificial intelligence and machine learning into research and clinical practices offers another promising avenue for advancements. These technologies could enhance predictive models that anticipate resistance patterns or response rates, thus optimizing treatment protocols before they are administered. Such integration could lead to dynamically informed therapeutic decisions that are continuously optimized to outpace the tumor’s evolution.
There is also a compelling case for diversifying clinical trial designs to include a broader range of demographic groups and real-world scenarios. Enhanced inclusivity would ensure that the benefits of combination strategies for NSCLC checkpoint inhibitors are accessible and effective for a wider patient population, reflecting true diversity and the varying impacts of environmental and genetic factors on treatment outcomes.
In conclusion, while the research spearheaded by Reyes, Muddasani, and Massarelli provides a foundational framework that significantly advances the landscape of NSCLC treatment, the expedition is far from over. The drive towards innovative research methodologies, coupled with a commitment to personalized and adaptive therapy regimes, will crucially dictate the trajectory of future successes. The comprehensive approach showcased in their research not only paves the way for upcoming advancements but also illuminates the path towards achieving longer and more resilient survival rates for NSCLC patients. The journey of refining **combination strategies for NSCLC checkpoint inhibitors** is evolving, promising a future where cancer’s complexity meets its match in the sophistication and precision of therapy strategies.